Connect With Us
Featured Articles

Ingrown Toenail Pain

Ingrown toenails occur when the edge of a toenail grows into the surrounding skin, leading to pain, redness or swelling, and sometimes infection. This condition is commonly caused by improper nail trimming, tight shoes, or toenail injuries. Initial treatment often includes soaking the foot in warm, soapy water to reduce inflammation and alleviate discomfort. Applying an over-the-counter antibiotic ointment and keeping the area clean can help manage infection. For more severe cases, a podiatrist might need to trim or remove part of the toenail and possibly prescribe medication to address infection or pain. To prevent future ingrown toenails, it’s important to cut toenails straight across and wear well-fitting shoes. Persistent or recurring ingrown toenails should be evaluated by a podiatrist. They can provide specialized care to relieve pain, treat infections, and offer advice on preventing future issues. If you have a problematic ingrown toenail, it is suggested you make an appointment with a podiatrist.
Ingrown toenails can become painful if they are not treated properly. For more information about ingrown toenails, contact Dr. Howard Horowitz of Bowie Foot & Ankle . Our doctor can provide the care you need to keep you pain-free and on your feet.
Ingrown Toenails
Ingrown toenails occur when a toenail grows sideways into the bed of the nail, causing pain, swelling, and possibly infection.
Causes
- Bacterial infections
- Improper nail cutting such as cutting it too short or not straight across
- Trauma to the toe, such as stubbing, which causes the nail to grow back irregularly
- Ill-fitting shoes that bunch the toes too close together
- Genetic predisposition
Prevention
Because ingrown toenails are not something found outside of shoe-wearing cultures, going barefoot as often as possible will decrease the likeliness of developing ingrown toenails. Wearing proper fitting shoes and using proper cutting techniques will also help decrease your risk of developing ingrown toenails.
Treatment
Ingrown toenails are a very treatable foot condition. In minor cases, soaking the affected area in salt or antibacterial soaps will not only help with the ingrown nail itself, but also help prevent any infections from occurring. In more severe cases, surgery is an option. In either case, speaking to your podiatrist about this condition will help you get a better understanding of specific treatment options that are right for you.
If you have any questions please feel free to contact our office located in Bowie, MD . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Ingrown Toenails
An ingrown toenail is a nail that has curved downward and grown into the skin. This typically occurs at either the nail borders or the sides of the nail. As a result, pain, redness, swelling, and warmth may occur in the toe. If a break in the skin forms due to the ingrown nail, bacteria may enter and cause an infection in the area; this is typically characterized by a foul odor and drainage.
Ingrown toenails have multiple reasons for developing. In many instances, the condition is a result of genetics and is inherited. The most common cause, however, is improper trimming; cutting the toenails too short forces the skin beside the nail to fold over. An ingrown toenail can also develop due to trauma, such as stubbing the toe, having an object fall on the toe, or participating in activities that involve repeated kicking or running. Wearing shoes that are too tight or too short can also cause ingrown toenails.
Treatment for an ingrown toenail varies between patients and the severity of the condition. In most cases, it is best to see your podiatrist for thorough and proper treatment. After examining your toe, your podiatrist may prescribe oral antibiotics to clear the infection if one is present. Surgical removal of either a portion of the nail or the entire nail may also be considered. In some cases, complete removal or destruction of the nail root may be required. Most patients who undergo nail surgery experience minimal pain afterward and can return to normal activity the following day.
Ingrown toenails can be prevented with proper nail trimming and by avoiding improper-fitting shoes. When cutting the toenails, be sure that you are cutting in a straight line and avoid cutting them too short. Shoes should not be too short or tight in the toe box.
Diabetic Foot Problems

Diabetic foot problems are primarily due to poor circulation and nerve damage caused by high blood sugar levels. This can lead to reduced sensation in the feet, making injuries and infections less likely to be noticed. Common foot problems can include ulcers, infections, and poor wound healing, which can escalate if not addressed promptly. The primary causes of diabetic foot issues are neuropathy, which reduces feeling in the feet, and peripheral artery disease, or PAD, which impairs blood flow. This combination can lead to minor injuries becoming serious infections, as the body's ability to heal is compromised. To manage and prevent diabetic foot problems, daily foot inspections are important. Look for cuts, blisters, or swelling, and report any abnormalities to your podiatrist. Proper foot hygiene is key. Wash and dry your feet thoroughly, and keep your toenails trimmed and clean. Wearing well-fitting shoes that offer support and protection helps to prevent injuries. To address any diabetic foot problems, it is suggested that you are under the care of a podiatrist who can regularly monitor your foot health.
Diabetic foot care is important in preventing foot ailments such as ulcers. If you are suffering from diabetes or have any other concerns about your feet, contact Dr. Howard Horowitz from Bowie Foot & Ankle . Our doctor can provide the care you need to keep you pain-free and on your feet.
Diabetic Foot Care
Diabetes affects millions of people every year. The condition can damage blood vessels in many parts of the body, especially the feet. Because of this, taking care of your feet is essential if you have diabetes, and having a podiatrist help monitor your foot health is highly recommended.
The Importance of Caring for Your Feet
- Routinely inspect your feet for bruises or sores.
- Wear socks that fit your feet comfortably.
- Wear comfortable shoes that provide adequate support.
Patients with diabetes should have their doctor monitor their blood levels, as blood sugar levels play such a huge role in diabetic care. Monitoring these levels on a regular basis is highly advised.
It is always best to inform your healthcare professional of any concerns you may have regarding your feet, especially for diabetic patients. Early treatment and routine foot examinations are keys to maintaining proper health, especially because severe complications can arise if proper treatment is not applied.
If you have any questions please feel free to contact our office located in Bowie, MD . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Diabetic Foot Care
Diabetes can cause two problems that can potentially affect the feet: Diabetic neuropathy and Peripheral Vascular Disease. Diabetic neuropathy occurs when nerves in your legs and feet become damaged, which prevents you from feeling heat, cold, or pain. The problem with diabetic neuropathy is that a cut or sore on the foot may go unnoticed and the cut may eventually become infected. This condition is also a main cause of foot ulcers. Additionally, Peripheral vascular disease also affects blood flow in the body. Poor blood flow will cause sores and cuts to take longer to heal. Infections that don’t heal do to poor blood flow can potentially cause ulcers or gangrene.
There are certain foot problems that are more commonly found in people with diabetes such as Athlete’s foot, calluses, corns, blisters, bunions, foot ulcers, ingrown toenails, and plantar warts. These conditions can lead to infection and serious complications such as amputation. Fortunately, proper foot care can help prevent these foot problems before they progress into more serious complications.
Each day you should wash your feet in warm water with a mild soap. When you finish washing your feet, dry them carefully especially between your toes. You should also perform daily foot inspections to ensure you don’t have any redness, blisters, or calluses. Furthermore, if you are diabetic, you should always wear closed-toed shoes or slippers to protect your feet. Practicing these tips will help ensure that your feet are kept healthy and away from infection.
If you have diabetes, contact your podiatrist if you have any of the following symptoms on your feet: changes in skin color, corns or calluses, open sores that are slow to heal, unusual and persistent odor, or changes in skin temperature. Your podiatrist will do a thorough examination of your feet to help treat these problematic conditions.
Bunion Complications

A bunion is a bony bump that forms on the joint at the base of the big toe, often causing the toe to deviate towards the others. Common issues can include chronic pain, bursitis or inflammation of the fluid-filled pads that cushion the bones, and metatarsalgia or pain and inflammation in the ball of the foot. Severe cases or complications can lead to hammertoes or crossover toes, where toes bend abnormally, and even arthritis in the big toe joint. Preventing bunion complications involves wearing properly fitted shoes with a wide toe box, avoiding high heels, and using orthotic inserts to reduce pressure on the bunion. Maintaining a healthy weight can also alleviate stress on the feet. Treatment options range from non-surgical methods like padding and medications to manage pain to surgical procedures for more severe cases. If you have a bunion that is causing worsening symptoms, it is suggested that you promptly consult a podiatrist who can help to manage symptoms and prevent further complications.
If you are suffering from bunion pain, contact Dr. Howard Horowitz of Bowie Foot & Ankle . Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is a Bunion?
Bunions are painful bony bumps that usually develop on the inside of the foot at the joint of the big toe. As the deformity increases over time, it may become painful to walk and wear shoes. Women are more likely to exacerbate existing bunions since they often wear tight, narrow shoes that shift their toes together. Bunion pain can be relieved by wearing wider shoes with enough room for the toes.
Causes
- Genetics – some people inherit feet that are more prone to bunion development
- Inflammatory Conditions - rheumatoid arthritis and polio may cause bunion development
Symptoms
- Redness and inflammation
- Pain and tenderness
- Callus or corns on the bump
- Restricted motion in the big toe
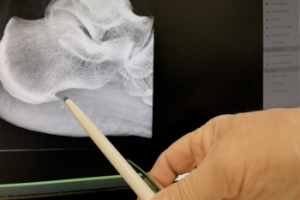
In order to diagnose your bunion, your podiatrist may ask about your medical history, symptoms, and general health. Your doctor might also order an x-ray to take a closer look at your feet. Nonsurgical treatment options include orthotics, padding, icing, changes in footwear, and medication. If nonsurgical treatments don’t alleviate your bunion pain, surgery may be necessary.
If you have any questions, please feel free to contact our office located in Bowie, MD . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Bunions
A bunion is a bump that forms at the base of the big toe. Bunions form when the big toe pushes against the next toe, which forces the big toe joint to get bigger and stick out. As a result, the skin over the bunion may start to appear red and it may feel sore.
There are risk factors that can increase your chances of developing bunions. People who wear high heels or ill-fitting shoes are more likely to develop them, in addition to those who have a genetic history of bunions or have rheumatoid arthritis.
The most obvious way to tell if you have a bunion is to look for the big toe pushing up against the toe next to it. Bunions produce a large protrusion at the base of the big toe and may or may not cause pain. Other symptoms are redness, swelling, and restricted movement of the big toe if you have arthritis.
Nonsurgical methods are frequently used to treat bunions that aren’t severe. Some methods of nonsurgical treatment are orthotics, icing and resting the foot, taping the foot, and pain medication. Surgery is usually only required in extreme cases. However, if surgery is needed, some procedures may involve removing the swollen tissue from around the big toe joint, straightening the big toe by removing part of the bone, or joining the bones of your affected joint permanently.
Your podiatrist will diagnose your bunion by doing a thorough examination of your foot. He or she may also conduct an x-ray to determine the cause of the bunion and its severity.
Symptoms and Prevention of Athlete’s Foot

Athlete's foot is a fungal infection that affects the skin on the feet, commonly caused by the fungus, trichophyton. Symptoms include itching, burning, and redness between the toes, along with peeling and cracking skin. In more severe cases, blisters and swelling may occur. Prevention is essential to avoid this uncomfortable infection. Keeping feet clean and dry is essential, as fungi thrive in moist environments. Wearing breathable, moisture-wicking socks and well-ventilated shoes helps reduce the risk. Avoiding walking barefoot in communal areas, such as locker rooms or swimming pools, can prevent exposure to the fungus. Regularly changing socks and practicing good foot hygiene further reduces the likelihood of becoming infected. Athlete’s foot can be uncomfortable and unsightly. If you have developed this fungal infection, it is suggested that you consult a podiatrist who can offer you effective treatment solutions, which may include prescribed medication.
Athlete’s Foot
Athlete’s foot is often an uncomfortable condition to experience. Thankfully, podiatrists specialize in treating athlete’s foot and offer the best treatment options. If you have any questions about athlete’s foot, consult with Dr. Howard Horowitz from Bowie Foot & Ankle . Our doctor will assess your condition and provide you with quality treatment.
What Is Athlete’s Foot?
Tinea pedis, more commonly known as athlete’s foot, is a non-serious and common fungal infection of the foot. Athlete’s foot is contagious and can be contracted by touching someone who has it or infected surfaces. The most common places contaminated by it are public showers, locker rooms, and swimming pools. Once contracted, it grows on feet that are left inside moist, dark, and warm shoes and socks.
Prevention
The most effective ways to prevent athlete’s foot include:
- Thoroughly washing and drying feet
- Avoid going barefoot in locker rooms and public showers
- Using shower shoes in public showers
- Wearing socks that allow the feet to breathe
- Changing socks and shoes frequently if you sweat a lot
Symptoms
Athlete’s foot initially occurs as a rash between the toes. However, if left undiagnosed, it can spread to the sides and bottom of the feet, toenails, and if touched by hand, the hands themselves. Symptoms include:
- Redness
- Burning
- Itching
- Scaly and peeling skin
Diagnosis and Treatment
Diagnosis is quick and easy. Skin samples will be taken and either viewed under a microscope or sent to a lab for testing. Sometimes, a podiatrist can diagnose it based on simply looking at it. Once confirmed, treatment options include oral and topical antifungal medications.
If you have any questions, please feel free to contact our office located in Bowie, MD . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Athlete’s Foot
Athlete’s foot, or tinea pedis, is a skin disease caused by a fungal infection. The infection typically occurs between the toes, and the feet are most subject to this disease because shoes best create the warm, dark, and moist environment in which fungus thrives. Other areas that create a similar environment, such as swimming pools, public showers, and locker rooms; can also promote fungi growth.
Symptoms of athlete’s foot include dry skin, itching, scaling, inflammation, and blistering. Sometimes, blisters can evolve into the cracks or breaks in the skin. The exposed tissue can then create pain, swelling, and discharge. The spread of infection can cause itching and burning as well.
While athlete’s foot commonly occurs between the toes, it may also spread to the toenails or soles of the feet. Other parts of the body, such as the groin or underarms, can also become infected if they are touched after the original area of infection is scratched. Aside from physical contact, athlete’s foot can also spread through the contamination of footwear, clothing or bedsheets.
Proper foot hygiene is essential in preventing athlete’s foot. You can prevent the fungus from spreading by frequently washing your feet using soap and water, thoroughly drying the feet between the toes, changing shoes and socks every day to reduce moisture, and ensuring that bathroom and shower floors are disinfected. Other tips include using shower shoes, avoiding walking barefoot in public environments, wearing light and airy shoes, and wearing socks that keep the feet dry.
While treatment for athlete’s foot can involve topical or oral antifungal drugs, mild cases of the infection can be treated by dusting foot powder in shoes and socks. Any treatment used can be supplemented by frequently bathing the feet and drying the toes. If proper foot hygiene and self-care do not ease your case of athlete’s foot, contact your podiatrist. He will determine if the underlying cause of your condition is truly a fungus. If that is the case, a comprehensive treatment plan may be suggested with the inclusion of prescription antifungal medications.
Understanding Heel Spurs
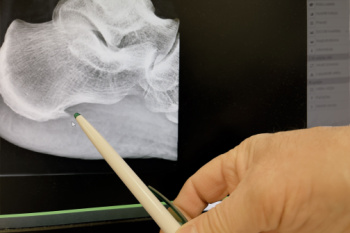
Heel spurs, medically termed calcaneal spurs, are bony outgrowths that develop on the underside of the heel bone. They often form in response to long-term inflammation and tension of the plantar fascia, which is the fibrous band of tissue that connects the heel to the toes. This condition, known as plantar fasciitis, is a common cause of heel spurs. Other factors contributing to heel spur formation include excessive strain on the feet from activities like running or standing for prolonged periods, obesity, and wearing poorly fitting shoes that lack adequate support. Diagnosing heel spurs typically involves a thorough physical examination by a podiatrist, focusing on symptoms like heel pain, especially upon waking or after long periods of rest. Imaging studies like X-rays may confirm the presence of a heel spur and help guide treatment options, which may include orthotics, stretching exercises, or in severe cases, surgery to alleviate symptoms. If you have heel pain, it is suggested that you consult a podiatrist who can provide an accurate diagnosis and proper treatment.
Heel spurs can be incredibly painful and sometimes may make you unable to participate in physical activities. To get medical care for your heel spurs, contact Dr. Howard Horowitz from Bowie Foot & Ankle . Our doctor will do everything possible to treat your condition.
Heels Spurs
Heel spurs are formed by calcium deposits on the back of the foot where the heel is. This can also be caused by small fragments of bone breaking off one section of the foot, attaching onto the back of the foot. Heel spurs can also be bone growth on the back of the foot and may grow in the direction of the arch of the foot.
Older individuals usually suffer from heel spurs and pain sometimes intensifies with age. One of the main condition's spurs are related to is plantar fasciitis.
Pain
The pain associated with spurs is often because of weight placed on the feet. When someone is walking, their entire weight is concentrated on the feet. Bone spurs then have the tendency to affect other bones and tissues around the foot. As the pain continues, the feet will become tender and sensitive over time.
Treatments
There are many ways to treat heel spurs. If one is suffering from heel spurs in conjunction with pain, there are several methods for healing. Medication, surgery, and herbal care are some options.
If you have any questions feel free to contact our office located in Bowie, MD . We offer the latest in diagnostic and treatment technology to meet your needs.